Chronic joint pain and depression are two of the most common health disorders, affecting millions of individuals worldwide. When these illnesses coexist, they produce a tough and complex situation that not only impacts physical well-being but also has a substantial impact on mental health and quality of life. Chronic pain and depression are more than just an undesirable pairing; they form a vicious cycle that is difficult to overcome.
In this article, we will look at how chronic joint pain and depression interact, how they affect the brain, and what efforts can be taken to control and relieve their symptoms.
Understanding Chronic Joint Pain.
Chronic joint discomfort lasts for months or even years. Osteoarthritis, rheumatoid arthritis, and autoimmune illnesses are common causes of joint inflammation and injury. Chronic joint pain causes a continual, often excruciating sense of agony, making daily actions like walking, sitting, and lifting objects more difficult.
Chronic joint pain is difficult to manage since it persists. Chronic pain, as opposed to acute pain, which is a transitory reaction to injury or sickness, lasts longer and is frequently unresolved. Over time, unremitting pain can cause changes in the neural system, resulting in increased pain sensitivity even in areas where there is no injury or inflammation. This phenomenon is known as central sensitization, in which the brain becomes more sensitive to pain signals.
Depression is more than simply feeling sad.

Depression is a mental health condition that affects a person’s feelings, thoughts, and actions. It is characterized by continuous unhappiness, pessimism, and a loss of interest or pleasure in formerly rewarding activities. People suffering from depression may also experience weariness, changes in appetite, and difficulties concentrating. Unlike transitory sadness, depression can endure for weeks, months, or even years without adequate treatment.
Many individuals are unaware that depression is more than simply a psychological condition; it also has serious consequences for the brain and body. The chemical imbalance theory of depression proposes that neurotransmitters including serotonin, dopamine, and norepinephrine regulate mood. When these molecules are out of balance, it can cause feelings of depression, hopelessness, and anxiety.
Furthermore, depression can affect brain structure and function. Depression has been proven in studies to decrease the hippocampus (a portion of the brain involved in memory and learning) and disturb the prefrontal cortex (which is in charge of decision-making, planning, and emotion regulation). These changes make it more difficult for people with depression to manage stress, stay motivated, and maintain a sense of well-being.
The Vicious Cycle: Chronic Pain and Depression Feed Each Other
Chronic joint pain and depression form a deadly feedback loop that is difficult to break. Chronic pain can lead to the development of depression, and sadness can increase the sense of pain, making it feel worse. Let’s look at how these two conditions reinforce each other.
Chronic pain causes depression:
Living in continual pain can be draining, both physically and mentally. As the pain continues, it might cause feelings of frustration, helplessness, and loneliness. People suffering from chronic joint pain may tend to believe that their agony defines their lives, which can lead to negative thought patterns and emotional turmoil. Over time, these sentiments might evolve into sadness, making the person feel stuck in a never-ending
Depression exacerbates pain:
Depression has the unique potential to alter our perception of pain. People who are depressed are typically more sensitive to physical experiences, including pain. This means that persistent joint pain can feel more severe when a person is depressed. Depression can also reduce pain tolerance, making it more difficult for people to deal with or control their physical symptoms.
Reduced Activity exacerbates both conditions.
Both chronic pain and depression can cause a decrease in physical activity. When people are in agony, they may postpone moving to avoid additional discomfort. However, inactivity can exacerbate pain and melancholy. Lack of exercise can stiffen the joints, causing more pain, and the isolation and inactivity that commonly accompany melancholy can make the sufferer feel worse emotionally. This lack of physical exercise also affects the release of endorphins, the body’s natural painkillers, which can make the pain feel worse.
Sleep Disruption:
Chronic pain and depression are both known to affect sleep. People with chronic pain may struggle to become comfortable enough to sleep comfortably, but those with depression may experience sleeplessness or hypersomnia. Poor sleep can increase both pain and depression symptoms, resulting in a never-ending cycle of discomfort, exhaustion, and mental anguish.
Impact on the Brain: How Pain and Depression Change Brain Function
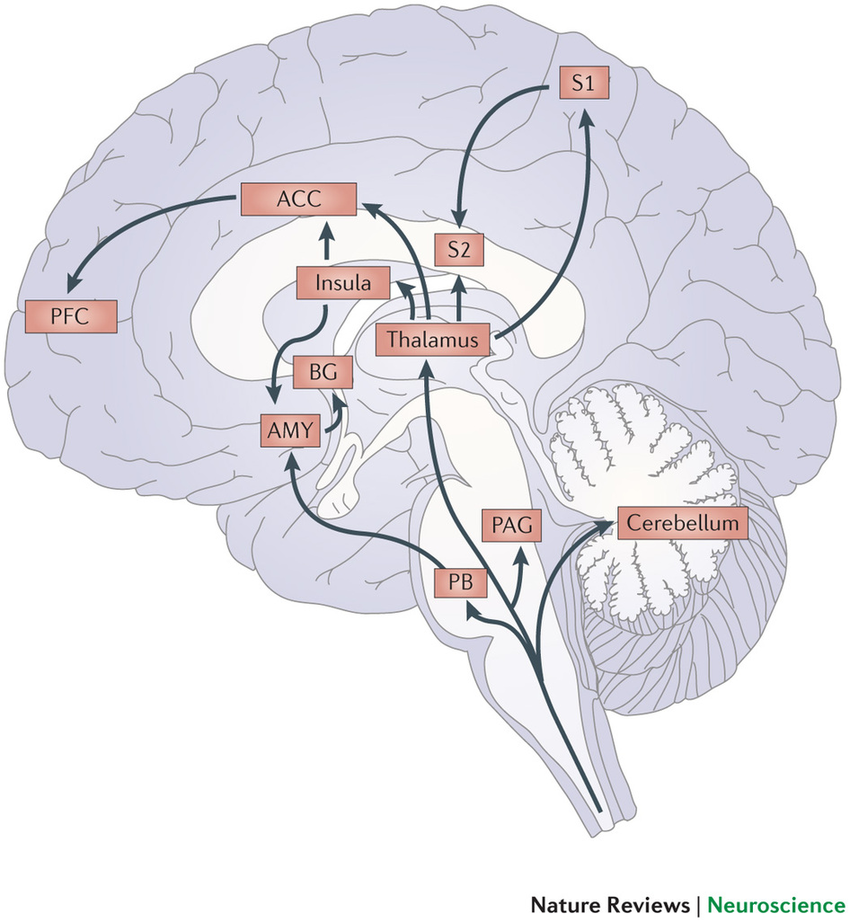
Chronic joint pain and depression have significant consequences on the brain. Studies have indicated that the brain areas responsible for pain processing and mood regulation are related. These overlapping pathways lead to the exacerbation of both pain and depression in people who suffer from both illnesses concurrently.
Increased Pain Sensitivity:
Chronic pain alters the brain’s pain-processing regions. This means that those with chronic pain may be more sensitive to pain signals. When depression enters the picture, the emotional anguish linked with unpleasant thoughts and feelings can exacerbate the impression of pain.
Changes in Brain Chemistry:
Both chronic pain and depression influence neurotransmitter levels in the brain. Chronic pain can cause the release of stress hormones such as cortisol, which over time can disturb the balance of neurotransmitters involved in mood regulation. Depression, on the other hand, is associated with abnormalities in serotonin, dopamine, and norepinephrine—chemicals involved in mood regulation and pain perception. Together, these elements produce a mental environment in which it is difficult to break free from either pain or despair.
Chronic pain and depression can both alter brain anatomy. For example, the hippocampus, which is involved in emotional regulation, memory, and pain perception, may decrease in both circumstances. This shrinkage can exacerbate the emotional and cognitive issues that people with chronic pain and depression confront, making it even more difficult for them to manage their symptoms.
Treatment Strategies: Breaking the Cycle
Managing chronic joint pain and depression necessitates a comprehensive approach that addresses both the physical and psychological elements of the illnesses. Here are some possible therapy options:
Medications:
Pain relievers:
Nonsteroidal anti-inflammatory medicines (NSAIDs), opioids, or corticosteroids can help relieve joint pain, but they should be used with caution, especially opioids, due to the danger of dependence.
Antidepressants:
such as selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs), can alleviate depressed symptoms by regulating neurotransmitter levels.
Cognitive Behavioral Therapy (CBT):
CBT is a very successful therapeutic strategy that assists people in rethinking negative thought patterns and developing coping skills for pain and sadness.
Physical therapy:
can assist persons with persistent joint pain maintain their mobility and function. Exercises designed to strengthen joints and reduce inflammation can help manage pain while increasing flexibility, minimizing physical restrictions caused by pain.
Mind-Body practices:
Mindfulness meditation, yoga, and relaxation practices can all help people manage pain and depression by encouraging relaxation, lowering stress, and increasing overall mental health. Mind-body techniques have been demonstrated to reduce pain perception and improve emotional regulation.
Lifestyle Changes:
Managing chronic pain and depression requires regular physical activity, a nutritious diet, and proper sleep hygiene. Staying active can cause the release of endorphins, which help with pain alleviation and mood improvement.
Conclusion
The combination of chronic joint pain and depression offers a significant difficulty for many people, affecting not just their physical health but also their mental well-being. The interaction of these two situations generates a deadly loop that sometimes seem impossible to break. Individuals can break this cycle and enhance their quality of life by implementing a comprehensive therapy plan that addresses both physical and mental health concerns. It is critical to seek professional assistance, whether through medication, therapy, or lifestyle modifications, in order to manage chronic pain and depression and recover control of one’s health and happiness.