The Link Between Panic Attacks and PTSD, Panic attacks. The sudden surge of overwhelming fear, the racing heart, the shortness of breath, the feeling of losing control. For many, these episodes are terrifying and isolating. While panic attacks can occur on their own, they are also significantly linked to Post-Traumatic Stress Disorder (PTSD), a condition that develops after a traumatic event. Understanding the complex relationship between panic attacks and PTSD is crucial for effective diagnosis, treatment, and ultimately, healing.
What are Panic Attacks?
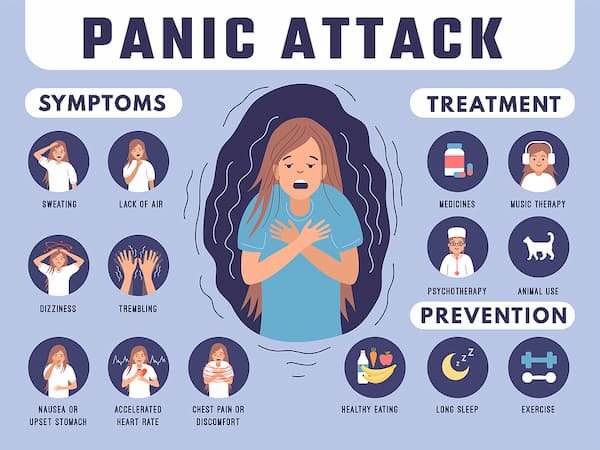
A panic attack is a discrete period of intense fear or discomfort, characterized by a range of physical and psychological symptoms. These symptoms can include:
- Physical: Palpitations, sweating, trembling, shortness of breath, chest pain, nausea, dizziness, chills or hot flashes, numbness or tingling sensations, feeling detached from reality (derealization), feeling like things around you aren’t real (depersonalization), fear of losing control or “going crazy,” and fear of dying.
- Psychological: Overwhelming anxiety, a sense of impending doom, a feeling of being trapped, and an intense urge to escape.
Panic attacks typically peak within minutes, leaving the individual feeling exhausted and shaken. While some people experience isolated panic attacks, others may develop panic disorder, characterized by recurrent attacks followed by persistent worry about having more attacks or their consequences.
What is PTSD?
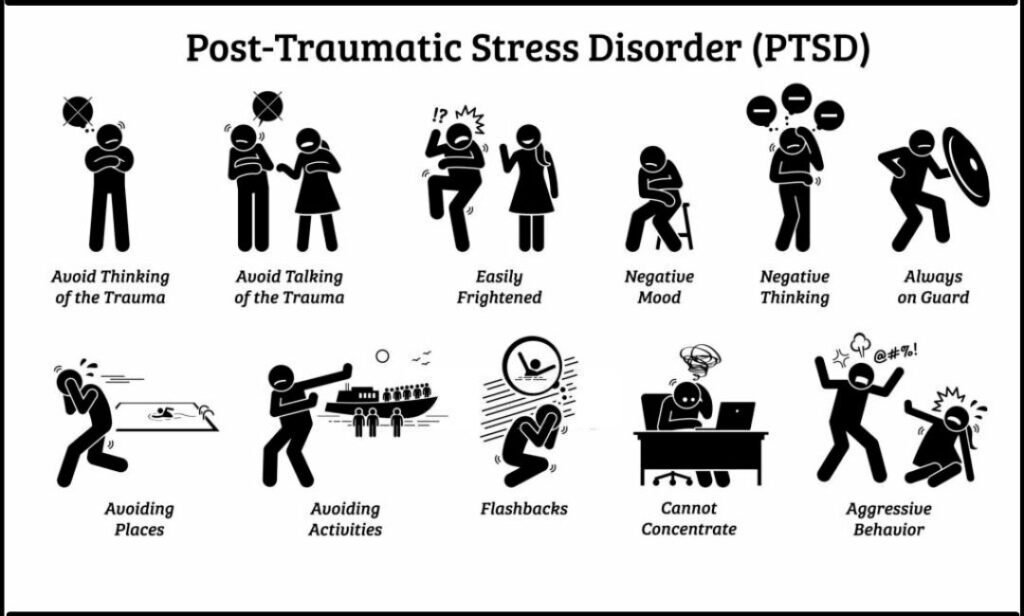
PTSD is a mental health condition that can develop after experiencing or witnessing a traumatic event, such as war, assault, natural disasters, or serious accidents. Individuals with PTSD often experience:
- Intrusion Symptoms: Recurrent, involuntary, and distressing memories of the traumatic event, flashbacks (reliving the event), nightmares, and intense psychological or physical reactions to reminders of the trauma.
- Avoidance: Persistent avoidance of stimuli associated with the trauma, including thoughts, feelings, places, people, or activities.
- Negative Alterations in Cognitions and Mood: Persistent and distorted sense of blame, negative emotional states (e.g., fear, anger, guilt, shame), diminished interest in significant activities, feeling detached or estranged from others, and inability to experience positive emotions.
- Alterations in Arousal and Reactivity: Irritability, reckless or self-destructive behavior, hypervigilance (being constantly on guard), exaggerated startle response, difficulty concentrating, and sleep disturbance.
The Overlap: Panic Attacks and PTSD
The connection between panic attacks and PTSD is multifaceted. Panic attacks can be a symptom of PTSD, occurring as part of the re-experiencing of the traumatic event. For example, a veteran might experience a panic attack triggered by a loud noise that reminds them of combat. In other cases, panic attacks can develop as a separate but co-occurring condition alongside PTSD. The chronic hyperarousal and anxiety associated with PTSD can make individuals more vulnerable to experiencing panic attacks, even in situations not directly related to the original trauma.
Key Differences:
While panic attacks and PTSD share some symptoms, there are important distinctions:
- Trigger: Panic attacks can sometimes appear to occur out of the blue, while PTSD symptoms are directly related to a traumatic event.
- Focus: In a panic attack, the focus is on the immediate physical and psychological symptoms of fear. In PTSD, the focus is on the traumatic event and its lasting impact.
- Duration: Panic attacks are typically short-lived, while PTSD symptoms can be chronic and persistent.
Why Does This Connection Exist?
Several factors contribute to the link between panic attacks and PTSD:
- Hyperarousal: Trauma can lead to a persistent state of hyperarousal, making individuals more sensitive to perceived threats and more likely to experience panic attacks.
- Emotional Dysregulation: PTSD can disrupt the ability to regulate emotions, making it harder to cope with anxiety and increasing the likelihood of panic attacks.
- Learned Associations: Individuals with PTSD may develop learned associations between certain triggers (e.g., a specific sound, smell, or place) and the traumatic event, leading to panic attacks in response to these triggers.
- Neurobiological Changes: Trauma can alter brain structures and neurotransmitter systems involved in fear and anxiety, increasing vulnerability to both panic attacks and PTSD.
The Importance of Diagnosis and Treatment
Recognizing the link between panic attacks and PTSD is essential for accurate diagnosis and effective treatment. A thorough assessment by a mental health professional can help determine whether panic attacks are related to PTSD or another condition.
Treatment Options:
Several effective treatments are available for both panic attacks and PTSD:
- Psychotherapy: Cognitive Behavioral Therapy (CBT), particularly exposure therapy and cognitive restructuring, is highly effective for both conditions. CBT helps individuals identify and challenge negative thoughts and beliefs, develop coping skills, and gradually confront feared situations.
- Medication: Medications, such as selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs), can be helpful in managing symptoms of both panic attacks and PTSD.
- Mindfulness-Based Therapies: Mindfulness practices can help individuals develop greater awareness of their thoughts and feelings, reducing the intensity of panic attacks and promoting emotional regulation.
- Support Groups: Connecting with others who have similar experiences can provide valuable support and reduce feelings of isolation.
Seeking Help:
If you are experiencing panic attacks or believe you may have PTSD, it is crucial to seek professional help. Early intervention and appropriate treatment can significantly improve your quality of life and help you regain control over your anxiety. Remember, you are not alone, and help is available. Reaching out is the first step towards healing and recovery. Don’t hesitate to contact a mental health professional, your doctor, or a crisis hotline for support and guidance. Taking care of your mental health is a sign of strength, and it is essential for your overall well-being.

