Understanding Borderline Personality Disorder, Borderline Personality Disorder (BPD) is a complex mental health condition that affects how individuals perceive themselves and others, often leading to emotional instability, relationship challenges, and impulsive behaviors. Despite its prevalence, BPD is frequently misunderstood, leading to stigma and barriers to effective treatment. In this comprehensive guide, we’ll explore the symptoms, causes, and treatment options for BPD, offering valuable insights for those affected and their loved ones.
What is Borderline Personality Disorder (BPD)?
Borderline Personality Disorder is a mental health condition characterized by intense emotional experiences, difficulty regulating emotions, and unstable relationships. It is classified as a personality disorder in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). People with BPD often struggle with self-image, fear of abandonment, and impulsive behaviors, which can significantly impact their daily lives.
While BPD can be challenging to manage, it is important to note that it is treatable. With the right support and treatment, individuals with BPD can lead fulfilling lives and build healthier relationships.
Symptoms of Borderline Personality Disorder
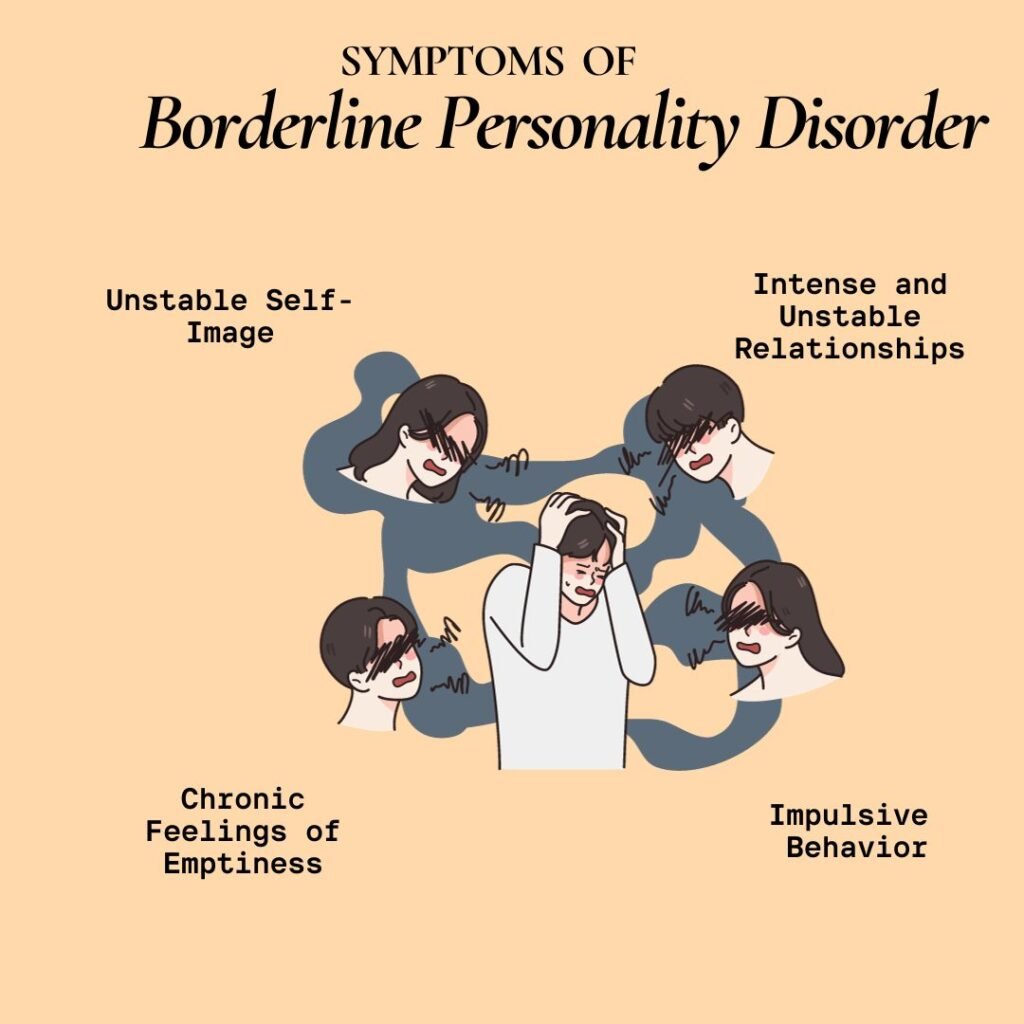
The symptoms of BPD can vary widely from person to person, but they generally fall into several key categories:
- Emotional Instability
- Intense mood swings that can last from a few hours to several days.
- Feelings of emptiness, sadness, or anger that are difficult to manage.
- Fear of Abandonment
- Extreme fear of being abandoned or rejected, often leading to frantic efforts to avoid real or perceived abandonment.
- Unstable Relationships
- Difficulty maintaining stable relationships due to alternating between idealization and devaluation of others (also known as “splitting”).
- Impulsive Behaviors
- Engaging in risky behaviors such as substance abuse, reckless driving, binge eating, or unsafe sexual practices.
- Self-Harm or Suicidal Behavior
- Recurrent thoughts of self-harm, suicidal ideation, or actual suicide attempts.
- Distorted Self-Image
- A persistently unstable sense of self, leading to frequent changes in goals, values, and aspirations.
- Chronic Feelings of Emptiness
- A pervasive sense of emptiness or boredom that is difficult to alleviate.
- Intense Anger
- Difficulty controlling anger, leading to frequent outbursts or physical fights.
- Paranoia or Dissociation
- Temporary episodes of paranoia or dissociation, often triggered by stress.
Causes of Borderline Personality Disorder
The exact cause of BPD is not fully understood, but research suggests that a combination of genetic, environmental, and neurological factors contribute to its development.
- Genetic Factors
- Studies indicate that BPD may have a hereditary component, as it is more common in individuals with a family history of the disorder or other mental health conditions.
- Brain Structure and Function
- Neuroimaging studies have shown that people with BPD may have differences in brain regions responsible for emotion regulation, impulse control, and decision-making.
- Environmental Factors
- Traumatic experiences, such as childhood abuse, neglect, or unstable family environments, are strongly linked to the development of BPD.
- Psychological Factors
- Certain personality traits, such as high sensitivity to stress or difficulty managing emotions, may increase the risk of developing BPD.
Diagnosis of Borderline Personality Disorder
Diagnosing BPD can be challenging due to the overlap of symptoms with other mental health conditions, such as bipolar disorder, depression, or post-traumatic stress disorder (PTSD). A mental health professional typically conducts a thorough assessment, including:
- A detailed interview to evaluate symptoms and their impact on daily life.
- A review of medical and psychiatric history.
- The use of standardized diagnostic criteria from the DSM-5.
Early diagnosis is crucial for effective treatment and improved outcomes.
Treatment Options for Borderline Personality Disorder

While BPD can be a lifelong condition, many individuals experience significant improvement with appropriate treatment. The most effective approaches often involve a combination of therapy, medication, and lifestyle changes.
- Psychotherapy
- Dialectical Behavior Therapy (DBT): Specifically designed for BPD, DBT focuses on teaching skills for emotion regulation, distress tolerance, and interpersonal effectiveness.
- Cognitive Behavioral Therapy (CBT): Helps individuals identify and change negative thought patterns and behaviors.
- Schema-Focused Therapy: Combines elements of CBT with other therapeutic approaches to address deeply ingrained patterns of thinking and behavior.
- Medication
- While there is no specific medication for BPD, certain medications can help manage symptoms such as mood swings, depression, or anxiety. These may include antidepressants, mood stabilizers, or antipsychotics.
- Hospitalization
- In severe cases, such as when there is a risk of self-harm or suicide, short-term hospitalization may be necessary to ensure safety.
- Lifestyle Changes
- Regular exercise, a balanced diet, and adequate sleep can help improve overall mental health.
- Mindfulness practices, such as meditation or yoga, can help manage stress and emotional regulation.
- Support Groups
- Joining a support group can provide a sense of community and understanding, helping individuals feel less isolated.
Living with Borderline Personality Disorder
Living with BPD can be challenging, but it is possible to manage symptoms and lead a fulfilling life. Here are some tips for individuals with BPD and their loved ones:
- Educate Yourself: Understanding BPD can help reduce stigma and improve self-awareness.
- Build a Support System: Surround yourself with supportive friends, family, and mental health professionals.
- Practice Self-Care: Prioritize activities that promote physical and emotional well-being.
- Stay Committed to Treatment: Consistency in therapy and medication is key to long-term management.
Breaking the Stigma Around BPD
BPD is often misunderstood and stigmatized, leading to feelings of shame and isolation for those affected. By raising awareness and promoting empathy, we can create a more supportive environment for individuals with BPD.
Conclusion
Borderline Personality Disorder is a complex but treatable condition that requires understanding, compassion, and effective treatment. By recognizing the symptoms, understanding the causes, and exploring the available treatment options, individuals with BPD can take meaningful steps toward recovery and improved quality of life.
If you or someone you know is struggling with BPD, seek help from a mental health professional. With the right support, it is possible to manage symptoms and build a life filled with hope and resilience.